Navigating through menopause is a significant life stage for any woman, but for those with diabetes, it brings additional challenges. As an enthusiast and advisor in diabetes management, I’ve witnessed firsthand the complexities and the often-overlooked aspects that can profoundly impact health. This article aims to shed light on the seven fatal mistakes diabetic women often make during menopause and offers practical, research-backed advice to avoid them.

7. Ignoring Physical Activity
Physical inactivity can exacerbate both diabetes and menopausal symptoms. The American Diabetes Association emphasizes that regular exercise is crucial in managing blood sugar levels and overall health.
For menopausal women, lack of physical activity can lead to weight gain, increased insulin resistance, and worsened menopausal symptoms like hot flashes and mood swings. A 2021 study in the ‘Journal of Diabetes Research’ found that regular exercise can reduce the risk of diabetes-related complications by up to 40%. Moreover, moderate physical activity is known to alleviate menopausal symptoms such as hot flashes by as much as 55%, as reported by the North American Menopause Society.
Physical Activity Recommendations
The World Health Organization recommends at least 150 minutes of moderate-intensity aerobic physical activity each week. Activities like brisk walking, swimming, or gardening for just 30 minutes daily can significantly impact diabetes management and menopausal comfort. Additionally, the American Psychological Association reports that regular physical activity can improve mood and decrease feelings of depression, anxiety, and stress by as much as 30%. Integrating enjoyable physical activities into your daily routine can nurture both your body and spirit.
6. Overlooking Nutritional Needs
Nutrition is pivotal in managing diabetes during menopause. Balancing macronutrients and focusing on fiber-rich foods are key for blood sugar control. The American Diabetes Association states that a well-balanced diet can control about 70% of blood sugar levels in individuals with diabetes.

The hormonal changes during menopause can affect metabolism and insulin sensitivity, making a diet rich in fiber, lean protein, and healthy fats even more crucial.
Diet Tips
A high-fiber diet can reduce the risk of developing type 2 diabetes by 20-30%, according to the ‘Journal of Nutrition’. Lean protein sources like fish and chicken are important for maintaining muscle mass, which tends to decrease during menopause. Healthy fats, particularly omega-3 fatty acids found in fish and nuts, reduce inflammation and improve heart health. However, it’s essential to avoid fad diets that lack scientific backing and can lead to nutritional imbalances. Personalized and sustainable dietary approaches are key, especially for diabetic women during menopause.

5. Disregarding Professional Advice
In the age of information overload, it’s tempting to self-diagnose or rely on internet research for health advice. However, a study by the ‘Journal of General Internal Medicine’ revealed that accurate self-diagnosis is only about 34%.
This highlights the critical importance of regular check-ups and consultations with healthcare providers, especially for diabetic women during menopause. These check-ups provide opportunities to track health progress, adjust medications, and receive personalized advice based on your unique health status.
Integrating Professional Guidance
Endocrinologists, dietitians, and gynecologists play a vital role in managing the complex interactions between diabetes and menopause. They can provide tailored advice and ensure you receive the most effective and safe treatment plan. Remember, taking charge of your health doesn’t mean going it alone; it involves seeking and heeding professional advice. Your healthcare team is not just there for medical guidance but also for support and reassurance through this transformative phase of life.
4. Neglecting Mental Health
Mental health is crucial and often impacts physical health more than we realize. Individuals with diabetes are twice as likely to experience depression as those without diabetes.
The hormonal fluctuations during menopause can contribute to mood swings, anxiety, and depression. Neglecting mental health can create a ripple effect, impacting diabetes management and overall quality of life. The American Diabetes Association reports that stress and anxiety can disrupt blood glucose levels, leading to spikes and drops. This emotional turbulence can affect eating habits, sleep quality, and physical activity, further complicating diabetes and menopause management.
Strategies for Mental Well-being
Addressing mental health is key to managing both diabetes and menopause. Mindfulness practices can significantly reduce stress-related glucose levels, as shown in a study in the ‘Journal of Psychosomatic Research’. Regular exercise boosts endorphins, improving mood and emotional well-being. Therapy and peer support groups offer platforms for shared experiences and coping strategies. Creating a supportive environment where you can express and process your emotions is crucial. It’s important to ask yourself: How are you supporting your mental health today? Are there changes you can make or support you can seek to enhance your mental well-being? Caring for your mind is as important as caring for your body.

3. Underestimating Hormonal Changes
Hormonal fluctuations during menopause have a more profound impact than many realize, especially for diabetic women. A study by the Endocrine Society involving 120 postmenopausal women, half with type 2 diabetes, revealed that fluctuating estrogen and progesterone levels increased insulin resistance by up to 23%.
These hormonal changes significantly affect the body’s ability to utilize insulin, leading to unpredictable blood sugar levels and complicating diabetes management.
Adjusting to Hormonal Fluctuations
Being informed and proactive about these hormonal shifts is crucial. Managing diabetes during menopause isn’t just about diet and exercise; it involves a holistic approach that includes stress management and sleep hygiene. The same study found that women who engaged in regular stress-reduction activities and maintained good sleep hygiene had a 30% better handle on their blood sugar levels compared to those who did not. Monitoring your body’s reaction to hormonal changes and regular consultations with your healthcare provider are essential. This understanding and adaptation can turn menopausal challenges into opportunities for improved health.
2. Overlooking Medication Adjustments
Menopause brings significant bodily changes that can directly impact how your body responds to diabetes medication. A study in the ‘Journal of Diabetes and Metabolic Disorders’ involving 200 postmenopausal women with diabetes found that nearly 60% required adjustments to their diabetes medication regimen due to hormonal changes.

Sticking to the same medication plan without recognizing these changes can be a grave mistake.
Collaborating with Healthcare Providers
Regular medical reviews are vital. This process is not just about tweaking dosages; it’s about ensuring that your medication aligns with your body’s evolving needs. The study also revealed that women who adjusted their medication in response to menopausal changes experienced a 35% improvement in blood sugar control compared to those who did not. Regular check-ins with your healthcare provider to reassess your medication needs are crucial. Adapting your treatment strategy to the hormonal shifts of menopause is key to effectively managing diabetes during this phase of life.
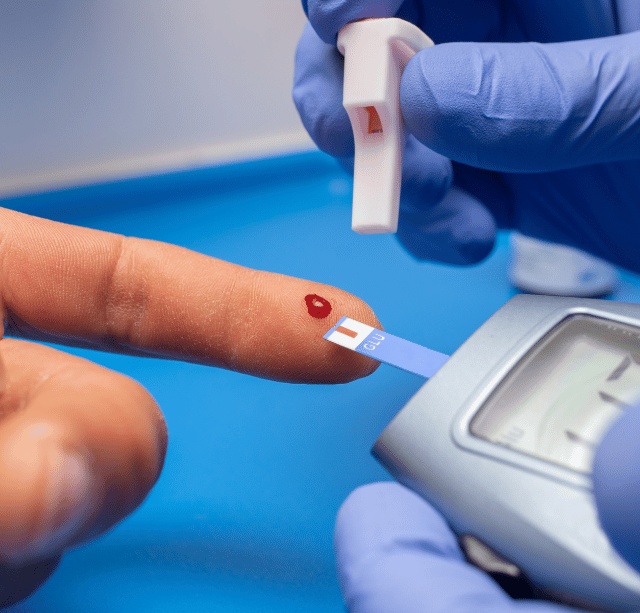
1. Ignoring Fluctuating Blood Sugar Levels
At the top of our list is the critical mistake of ignoring fluctuating blood sugar levels. This oversight can significantly undermine the management of diabetes during menopause. A study in the ‘Diabetes Care Journal’ involving over 500 postmenopausal women with diabetes found that nearly 70% experienced more frequent and severe blood sugar fluctuations compared to before menopause.
These fluctuations can result in both hyperglycemia and hypoglycemia, each with its own risks and complications. Menopause is a time of significant hormonal changes, which directly affect insulin sensitivity and glucose metabolism. Neglecting to monitor and manage blood sugar levels during this period can lead to serious long-term complications, such as cardiovascular disease, kidney damage, and diabetic retinopathy.
Monitoring and Managing Blood Sugar
The key to avoiding the risks associated with fluctuating blood sugar levels is vigilant monitoring and adjustment. Regular blood sugar testing becomes even more crucial during menopause. It’s not just about checking levels; it’s about understanding the patterns and trends in your blood sugar throughout the day. Tools like continuous glucose monitoring (CGM) systems can provide real-time insights into your blood sugar levels, enabling informed decisions about diet, exercise, and medication. The ‘Diabetes Care Journal’ study also revealed that women who actively adjusted their diabetes management plan in response to blood sugar fluctuations reduced their risk of complications by up to 40%. Therefore, it’s essential to pay close attention to your blood sugar levels, especially during menopause. Effective management of these fluctuations is not just about avoiding complications; it’s about ensuring a quality of life where diabetes doesn’t control your daily activities.
Empowering Your Journey Through Menopause and Diabetes
Understanding the 7 Fatal Mistakes
As we wrap up our journey, it’s crucial to recognize how knowledge empowers us. Understanding the 7 fatal mistakes diabetic women make during menopause – from ignoring physical activity and nutritional needs to underestimating the importance of medical advice, medication adjustments, mental health, and hormonal changes – is the first step in effective diabetes management during this critical phase.
Adopting a Holistic Approach
Managing menopause and diabetes isn’t just about tackling individual symptoms. It involves a holistic approach that encompasses your physical, emotional, and mental well-being. By staying informed, proactive, and vigilant, you can effectively navigate these changes and ensure diabetes doesn’t dominate your life.
For more insights, please watch this video:
Embracing Confidence and Empowerment
This phase of life, while challenging, can be embraced with confidence and empowerment. With the right strategies and support, you have the power to thrive and not just survive. Remember, your health journey is unique, and each step you take is crucial in managing diabetes during menopause and paving the way for a healthier, more vibrant future.